In advance of the announcement of an expected provincial lockdown on Thursday (April 1), Ontario’s top health officials delivered a sobering assessment of the status of the COVID-19 pandemic in Ontario — and recommended a month-long province-wide stay-at-home order to bring the disease under control.
“We are in the third wave of the pandemic and, as the new variants spread, you will see that COVID is killing faster and younger,” said Adalsteinn Brown, co-chair of Ontario’s COVID-19 science advisory table, who presented COVID-19 modelling projections along with chief medical officer of health Dr. David Williams.
“It’s spreading far more quickly than it was before, and we cannot vaccinate quickly enough to break this third wave,” Brown added.
Brown described the situation in Ontario’s hospitals now, compared to the first and second waves of the pandemic.
“It used to be that one family member, often an older parent or grandparent, would be in an intensive care unit while other members of the family would have caught a much milder form of the disease if at all,” he said. “But with the new variants, that are both more contagious and more dangerous, we’re seeing situations where whole families end up in intensive care, all at the same time.”
Brown added that, because Ontario’s health care system is already under strain, patients have to moved between regions.
“Even as people are fighting for their lives, we have to separate families,” he said. “One family ended up spread between three hospitals … another family ended up being spread between three cities, in three different hospitals, and all of them died.”
Brown pointed out that the variants of concern are resulting in younger people ending up in hospital, using the example of one physician’s observations.
“This doctor worked through the brunt of the first and second wave,” Brown said. “He told us very clearly that even at the worst of these times, he hadn’t seen this many young otherwise healthy people fighting for their lives against COVID-19.”
While vaccination is the key to long-term control, Brown said, adherence to public health measures — masks, physical distancing, hand hygiene, and staying outside if you need to meet people — are key to controlling the pandemic while people are being vaccinated.
“Sometimes we talk about public health measures and the economy, or public health measures and mental health, as a trade-off,” Brown said. “This is a false debate. The faster we get the pandemic under control, the faster we return to normal. Partial measures, half-hearted adherence, and denial prolong the pandemic and make life harder for everyone.”
Brown said this was particularly true for children and youth, with school infections reflecting what is happening in the community.
“Schools should be the last place to close, and the first to open,” Brown said.
“But as international experience shows, if we don’t get the pandemic under control, we will have to take more drastic measures for longer periods of time. If we don’t get the pandemic under control, we’ll have more sick people, some of whom will never get better. We will further damage our hospital system and the people working in it. We’ll have more unnecessary death, and it will hurt students and our society.”
Brown then presented an update on COVID-19 modelling projections, that included the following key findings:
- The third wave is here and being driven by variants of concern.
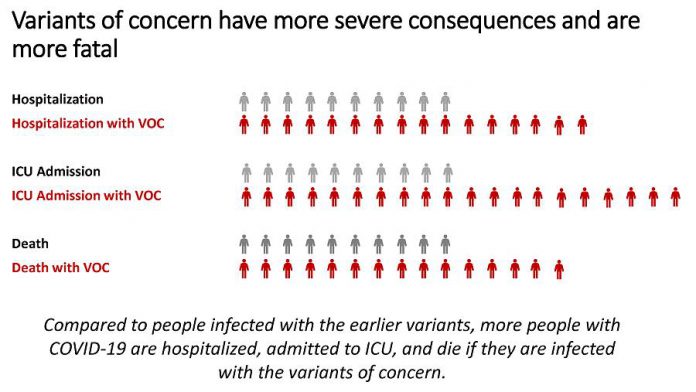
- Younger Ontarians are ending up in hospital. With the UK B.1.1.7 variant, the risk of ICU admission is two times higher and the risk of death is 1-1/2 times higher.
- COVID-19 threatens the health system ability to deal with regular ICU admissions and the ability to care for all patients.
- Vaccination is not reaching the highest-risk communities, delaying its impact as an effective strategy.
- School disruptions have a significant and highly inequitable impact on students, parents and society. Further disruptions should be minimized.
- Stay-at-home orders will control the surge, protect access to care, and increase the chance of the summer Ontarians want.
Other points raised during the presentation include:
Cases and positivity rates in most public health unit regions now exceed the criteria for them to be placed in the ‘Red-Control’ level of Ontario’s COVID-19 response framework.
The increase in cases is not the result of more testing, because testing rates have remained flat.
Most new cases are variants of concern and, compared to people infected with the earlier variants, more people with COVID-19 are hospitalized, admitted to ICU, and die if they are infected
with the variants of concern.
Short-term projections are for 6,000 cases per day by the end of April, unless there is a province-wide stay-at-home order. While either a two-week or four-week stay-at-home order will reduce daily cases to below 2,000, a two-week stay-at-home order will result in cases creeping back up to 2,000 by the end of the month.
With a stay-at-home order in place, ICU occupancy will peak at 800 beds by the end of April, and then gradually decline. Without a stay-at-home order, ICU occupancy will reach 1,000 beds. In either case, hospitals may have to begin triaging patients to manage the burden on the system.
The cumulative surgical backlog related to the pandemic has now affected 245,367 patients, with urgent surgeries making up the majority of these cases.
Essential workers, particularly racialized and marginalized communities in urban centres, are bearing the brunt of the pandemic, making vaccination of essential workers and control of workplace outbreaks critical.
While vaccinations of older Ontarians are continuing, a large percentage of them have still not received a first dose, including 17 per cent of those 80 and older, 40 per cent of those 75 to 79, and 72 per cent of those 70 to 74. Fewer older Ontarians in high-risk neighbourhoods have received vaccinations compared to more older Ontarians in low-risk neighbourhoods who have received vaccinations.
School interruptions will have significant impacts on students, families, and society. Students whose learning is interrupted by the pandemic will experience a drop in lifetime earnings and face health risks from social isolation and loss of structure, with students who are already disadvantaged being affected more.
PDF: Update on COVID-19 Projections – Ontario’s Science Advisory and Modelling Consensus Tables – April 1, 2021
Update on COVID-19 Projections - Ontario's Science Advisory and Modelling Consensus Tables - April 1, 2021
A copy of this PDF is available from covid19-sciencetable.ca.